The 5 Most Common Eye Injuries for Athletes
Sports and physical activities play a crucial role in maintaining a healthy lifestyle, but they also come with potential risks, including eye injuries

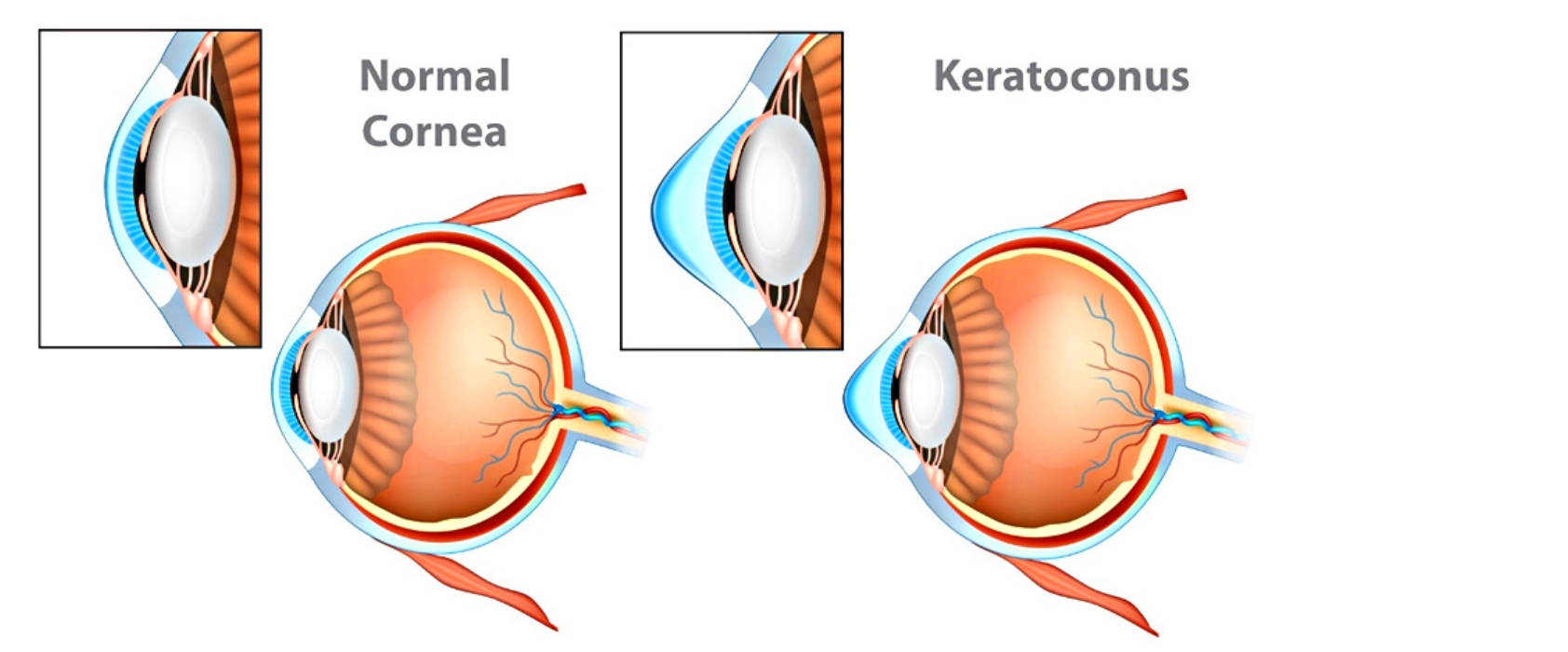
Keratoconus is an inherited condition of the cornea (the transparent front surface of the eye), where the normally round cornea becomes thinned, distorted and coned-shaped.
The cornea is important to our eyes for a number of reasons. The cornea is the outermost layer of the eye, which contains five layers of membranes that each have different functions. All five layers help to protect the rest of the eye from dirt, bacteria, and other substances that our eyes might come into contact with throughout the day.
Our corneas also play a significant role in the refractive process of our eyes, focusing 65-75% of the images that we see. Without this refractive process that takes place in the corneas, the images that we see would become blurry. With keratoconus, this abnormal shape of the cornea prevents the light entering the eye from being focused correctly on the retina and causes distortion of vision. For this reason, patients with this condition often experience distorted vision which makes everyday tasks like driving, reading, or typing difficult.
Keratoconus symptoms range from mild to severe. Signs and symptoms of keratoconus may change as the disease progresses. They include:
Keratoconus does not discriminate, it affects people of all races and both sexes. Typically this condition develops during the individual’s teenage years, progresses through the 20s and usually stops progressing after the age of 30. Since is it common for there to be a family history of the disease, about 1 out of 10 people with keratoconus have a parent who has it too.
Risk Factors
While eye care professionals do not know for sure what causes keratoconus, there are several risk factors which can increase your chances of developing this condition, which includes:

While there are several different surgical and nonsurgical options to treat and stop the condition from further development, there is no way that you can prevent this condition as such. The best thing you can do to help decrease the severity and prevent it from getting worse is not to rub your eyes and seek treatment as soon as possible.
Keratoconus treatment depends on the patient’s symptoms and how quickly the condition is progressing. When the symptoms are mild to moderate, the patient’s vision can often be corrected with eyeglasses or soft contact lenses. For most people with keratoconus, the cornea will become stable after a few years. If you have this type, you likely won’t experience severe vision problems or require further treatment.
Other non-surgical treatments option include:
Hard Contact Lenses
As keratoconus gets worse, vision may no longer be correctable with glasses because of the amount of irregular astigmatism. Therefore to correct the patient’s vision, he/she may need to be fitted with a special type of hard gas permeable contact lenses.
In most cases, these rigid gas permeable contact lenses are adequate but they require frequent check ups and must be carefully fitted by an optometrists. Lens changes may be needed to achieve and maintain good vision.
Piggyback lenses
If the patient finds rigid lenses to be uncomfortable, the ophthalmologist or optometrist may recommend “piggybacking” a hard contact lens on top of a soft one as an alternative. Although it takes more work to put on each day with an extra step, some patients find this dual lens system prevents the rigid lens surface from irritating the sensitive cornea.
Hybrid lenses
These speciality contact lenses incorporate a GP (gas permeable) lens and have a rigid center with a softer ring around the outside for increased comfort. People who can’t tolerate hard contact lenses may prefer hybrid lenses.
Scleral lenses
These lenses are useful for very irregular cornea shape changes in advanced keratoconus. Scleral lenses are larger than regular contact lenses and are designed to vault over the entire cornea and rest on the sclera (the white part of the eye). Because of the size, the lens bowl must be filled with non-preserved saline before being placed on the eye.
Instead of resting on the cornea as traditional contact lenses do, scleral lenses sit on the sclera and vault over the cornea without touching it. While many patients initially find applying and removing scleral lenses challenging, the majority achieve exceptional vision and comfort.
Surgery:
For some patients the cornea can become scarred, making if difficult to wear contact lenses. In this instance, surgery may be necessary. Surgical procedures designed to treat more severe cases of keratoconus include:
If you are having difficulty with your vision and suspect you or your loved one may have keratoconus, we recommend you book an appointment at Auckland Eye. Here at Auckland Eye, we have most advanced technology and equipment to treat keretoconus and accurately determine the topography (shape and thickness) of the cornea, which allows us to screen for potential keratoconic changes to the eye. We offer the highest quality of care as each ophthalmologist has international and specialist training in specific eye diseases and surgery techniques to provide the best possible visual outcomes for all of our patients.

Sports and physical activities play a crucial role in maintaining a healthy lifestyle, but they also come with potential risks, including eye injuries

For those leading an active lifestyle or engaged in sports, the significance of clear vision cannot be overstated.

Uncover the revolutionary technology behind LASIK that has empowered millions to enjoy clear vision without glasses.