Understanding Keratoconus
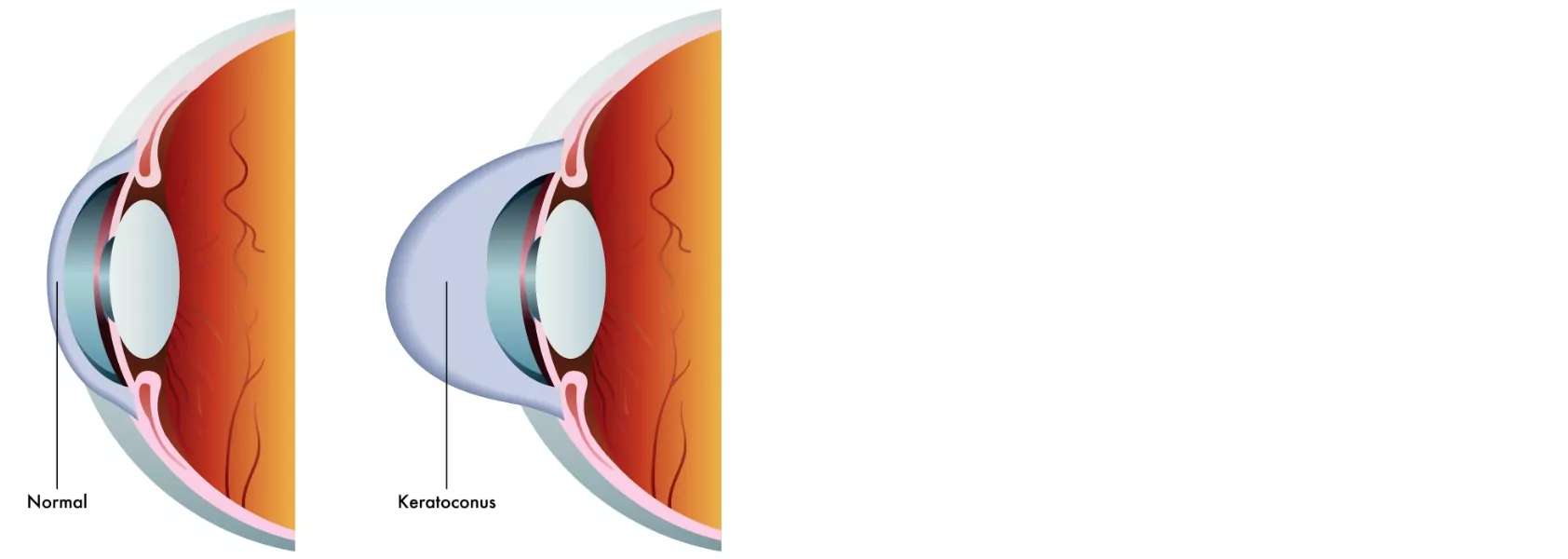
Keratoconus is a genetic disease that gradually warps the shape of the cornea – the transparent front surface of the eye – into a pointed, cone-like shape. As a result, vision becomes distorted. Keratoconus sufferers are usually very near-sighted, with astigmatism that is difficult to correct with glasses or contacts.
If you think you may have keratoconus, talk to your ophthalmologist for advice and treatment options.
Causes and progression
Keratoconus usually starts in the late teens or early twenties, causing slight blurring of vision and light sensitivity. The cornea continues to change for 10 to 20 years, with vision becoming worse over that time. When the cornea stops changing, vision stabilises but will not return to normal.
Keratoconus can have a different effect on each eye, with mild vision issues in one eye and severe distortion in the other.
Risk factors
- Family history – keratoconus has a strong genetic link, affecting around 50% of patients’ family members.
- Down syndrome – the disease is more common in people with Down syndrome.
- Other conditions – keratoconus has been linked to a range of health conditions, including hay fever, eczema and asthma.
Symptoms
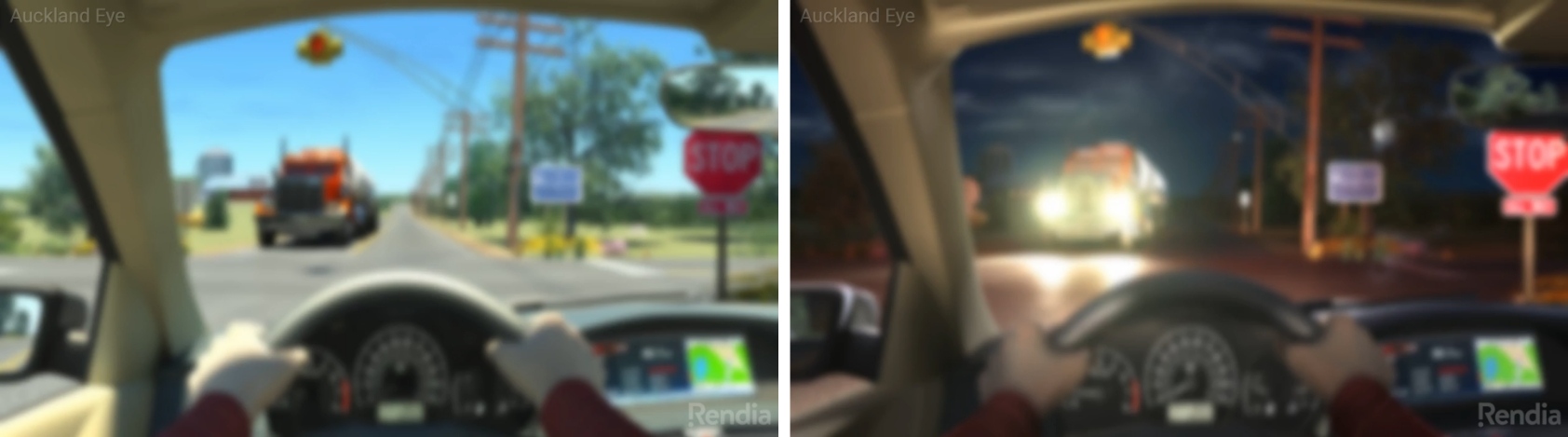
Because keratoconus progresses so slowly, it can be difficult to identify early.
Symptoms may include:
- Near-sightedness
- Astigmatism
- Blurred vision that isn’t resolved by contacts or glasses
- Light sensitivity (photophobia)
- Glare at night
- Frequent eye rubbing
- Constant prescription changes for glasses or contacts
Diagnosis
Your ophthalmologist will diagnose keratoconus with an eye exam, possibly using a slit lamp to examine the cornea and check for changes in shape. Later, you may need an ultrasound of the eye.
Hydrops and keratoconus
In some people, keratoconus can lead to a secondary condition called hydrops. The misshapen cornea develops a tiny split on the inner surface, causing sudden swelling and vision problems. The split may take weeks or months to heal, and as it does, scar tissue will build up in its place.
While most find that the scar tissue worsens vision, occasionally, it does the opposite, enhancing the shape of the damaged cornea and improving vision.
If you have keratoconus and experience sudden swelling and loss of vision, seek urgent help from your ophthalmologist or doctor. Although there’s no cure for hydrops, you may be prescribed eye drops to relieve any pain or discomfort.

Treating keratoconus
Although there’s no way to restore the cornea to its original shape, there are ways to slow or halt the disease’s progression.
Your treatment will depend on how early keratoconus is diagnosed and how severely it affects your vision.
Treating myopia and astigmatism associated with keratoconus is the first step. However, glasses and contacts can’t reshape the cornea – they can only treat vision issues. Once these become impossible to treat with glasses or contacts, it may be time for surgery.
Glasses and soft contact lenses – in the early stages, ordinary glasses or contact lens prescriptions should be able to correct vision issues.
Hard contacts may be a better option as the condition progresses. This type of contact lens needs to be fitted by an optometrist, and the prescription may need to be updated frequently. Note: you may be able to access a government subsidy to help with the cost of contact prescriptions.
Corneal collagen cross-linking
If your keratoconus is still progressing, you may be a candidate for a surgical procedure called corneal collagen cross-linking, designed to halt the progression of the disease and stabilise your vision before it worsens.
During the procedure, the surgeon directs ultra-violet (UV) light toward the affected cornea. The tissue produces bonds between collagen fibres, strengthening the framework of the cornea and preventing further distortion.
Recovery
The cross-linking procedure takes about an hour, and you will usually be able to go home on the same day. With incisions, recovery is usually straightforward.
Corneal implants
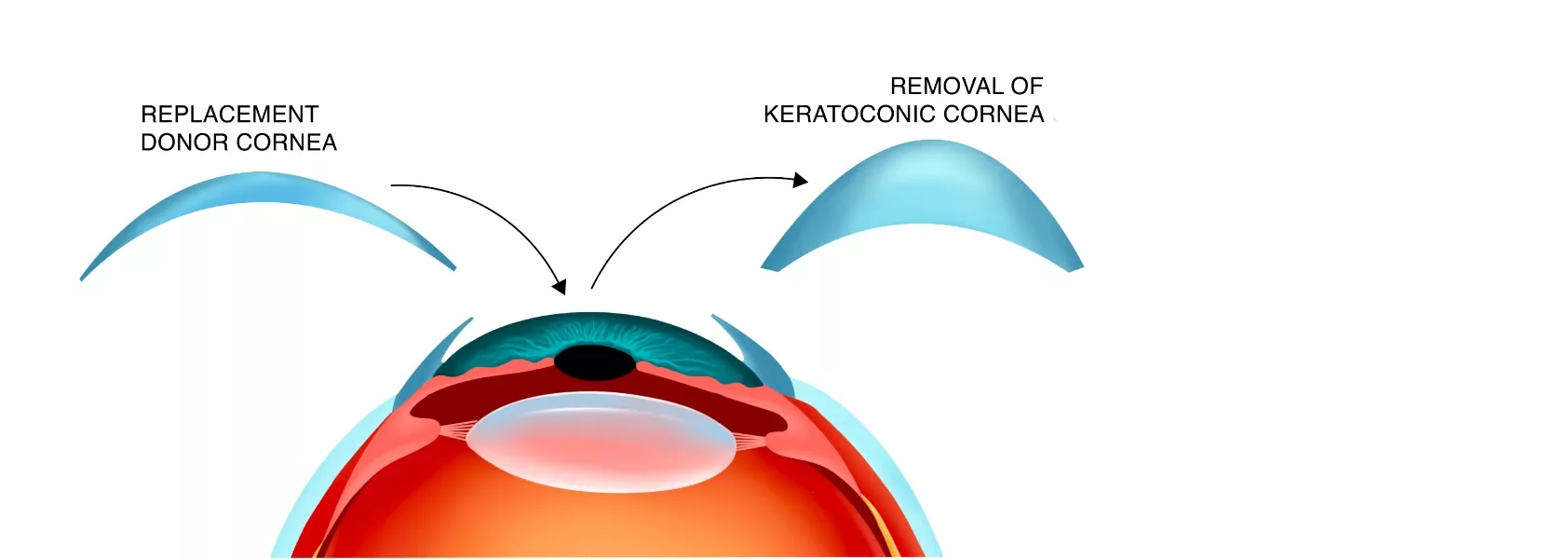
If your keratoconus is too severe for cross-linking and your vision issues are not responding to glasses or contacts, a corneal transplant may be the only option. This surgical procedure involves removing the cone-shaped cornea and replacing it with a cornea from a carefully selected donor.
Recovery
Corneal transplants are done under general anaesthetic. You may be able to go home on the day of the procedure, but you will need someone to drive you. A long period of post-operative care will ensure the grafted tissue stays healthy. You will also need to take time off work for recovery – two to three weeks for many jobs and three to four months for jobs that involve heavy lifting or manual labour.