Understanding uveitis
Uveitis is an umbrella term for inflammation of the inner eye. Uveitis ranges from mildly irritating to severe and potentially harmful. Many cases are ongoing or recurring, so treatment is aimed at keeping symptoms and eye damage under control. Severe cases can cause vision loss if left untreated.
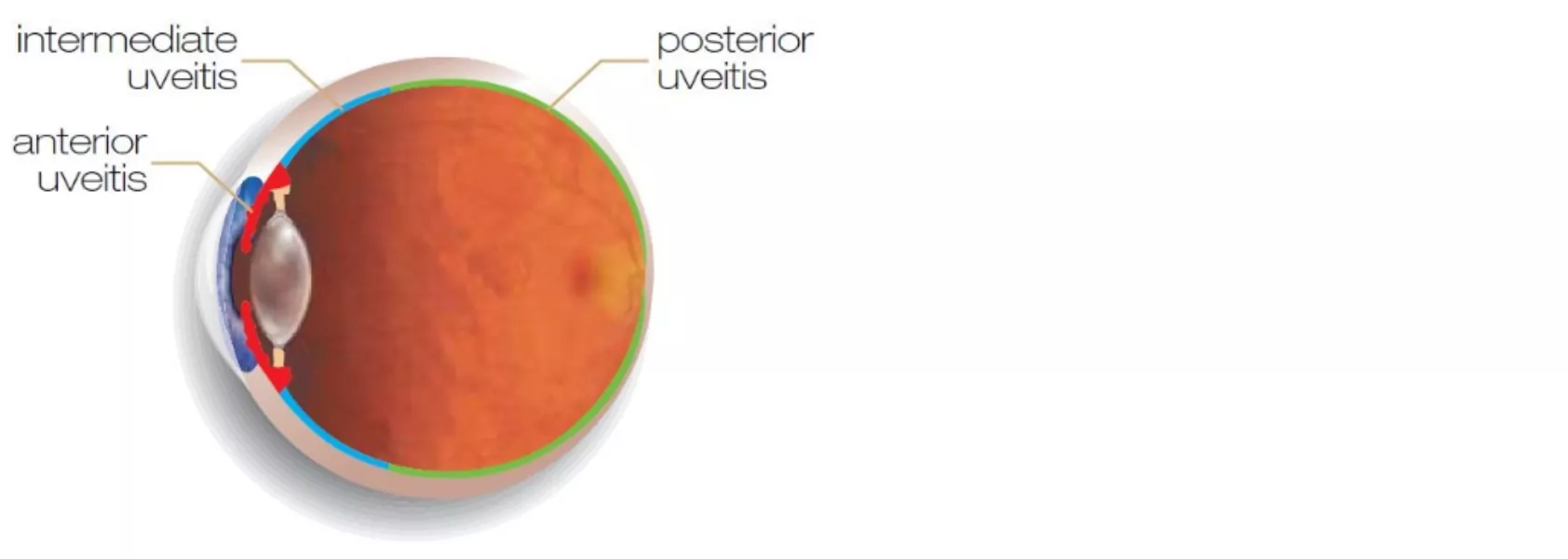
Types of uveitis
There are several forms of uveitis, depending on which part of the uvea is infected.
Anterior uveitis – iritis
The most common type of uveitis starts in the iris – although the ciliary body may also be inflamed in some cases.
Intermediate uveitis
This form of uveitis involves inflammation behind the ciliary body. Because this area is close to the back of the eye, the retina may also become inflamed.
Posterior uveitis
This serious subtype affects the back of the eye, which includes the retina. Blood vessels around the retina and the retina itself can become inflamed, making it a potential threat to your vision.
Panuveitis
This affects all parts of the uvea and can spread through the entire eye. Like posterior uveitis, it’s a serious issue that needs quick treatment.
Identifying uveitis
Because uveitis comes in so many forms, symptoms can vary significantly. In most cases, symptoms will only appear in one eye.
Common symptoms:
- Redness in the eye
- Light sensitivity (photophobia)
- Aching or pain in the affected eye
- Blurred vision
- Increased floaters (dark or transparent shapes that drift through your vision)
- A smaller pupil in the affected eye
If you are concerned about uveitis symptoms, talk to your ophthalmologist as soon as possible.
Diagnosis
Diagnosing uveitis involves a standard eye exam, imaging and other tests if required.
Causes and risk factors
Uveitis can occur in people with no eye issues or other health problems. However, there are risk factors:
- History of uveitis
- Arthritis or psoriasis
- Any infection – bacterial, viral, parasitic or fungal
- Genetics – a gene called HLA-B27 is present in the majority of uveitis sufferers
- Inflammatory bowel disease
- While uveitis primarily stems from issues or illnesses within the eye, it may also have associations with various autoimmune and inflammatory conditions. Examples include inflammatory bowel diseases (IBDs) such as Crohn’s disease and ulcerative colitis. Notably, IBD extends beyond the gastrointestinal (GI) tract, manifesting in extraintestinal symptoms that affect various parts of the body, including the eyes.

Treatment options
Completely resolving uveitis can be difficult, so most treatment focuses on minimising pain and inflammation and protecting your vision. If caused by an infection, it may be resolved with antibiotics.
Corticosteroid eye drops
Iritis can be treated with steroidal eye drops, which may be needed for several weeks.
Steroid injections
If uveitis is present inside the eye, corticosteroid injections may be required.
Steroid tablets
Panuveitis or posterior uveitis may be treated with oral steroids rather than injections.
Intravenous steroids
If your uveitis is threatening your vision, intravenous steroids may be used to deliver medication to the affected eye as quickly as possible.
Immunosuppressants
If your uveitis is linked to an inflammatory condition, immunosuppressants help keep inflammation and pain under control.
Mydriatic eye drops
Alongside corticosteroids and other medications, these eye drops help relieve pain and prevent further eye damage.

Recovery and recurring uveitis
Iritis may resolve in four to six weeks with appropriate treatment. Forms of uveitis that affect the inner eye can take much longer – in some cases, becoming a chronic condition that requires long-term medication.
Recurring uveitis is also common, so it’s important to watch for symptoms after the initial case has been resolved.







