Understanding macular degeneration
Macular degeneration, also called age-related macular degeneration (AMD), is one of the most common causes of vision deterioration in older people. It’s estimated to affect around 15% of people over 50 and 30% of those aged 75+.
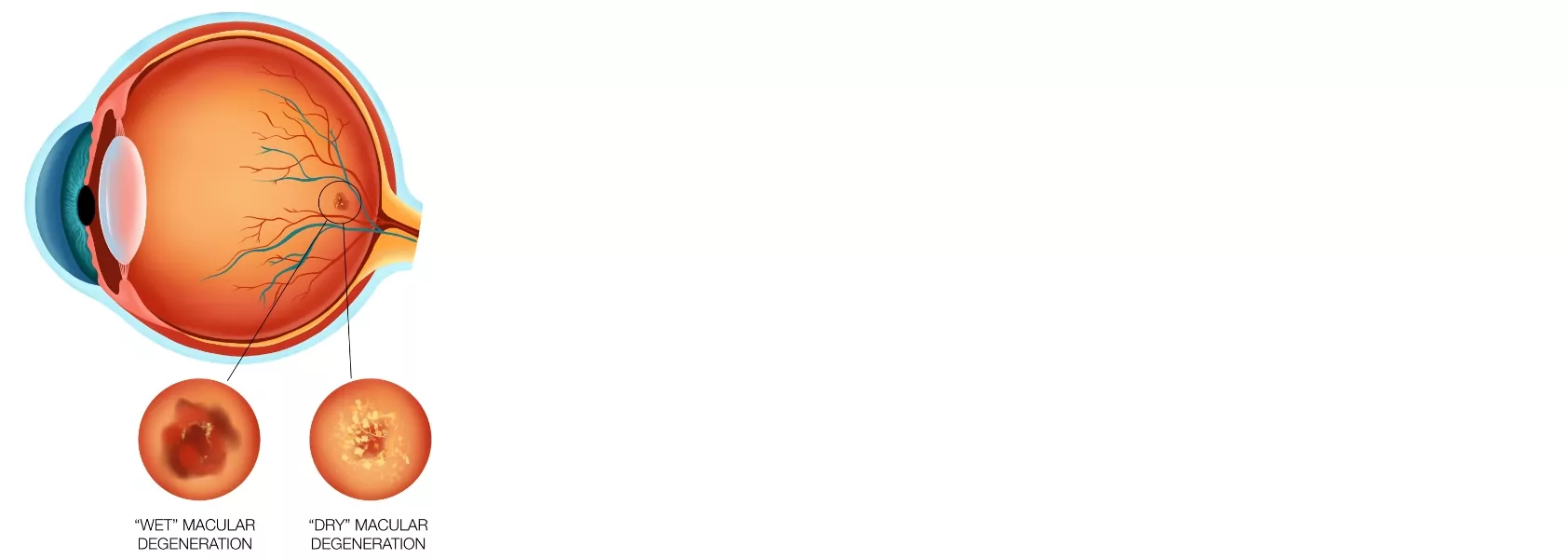
The condition affects the macula – the sensitive central section of the retina responsible for transmitting detail and colour images to the brain. As the macula declines over time, the central field of vision is affected, and colour vision may deteriorate.
This video describes AMD as the deterioration of the center of the retina, or macula, with a further description of the macula’s function. Describes early to late stage symptoms, showing how central vision becomes increasingly blurry and dark, while side vision remains unaffected. Urges patients to have regular check-ups to maintain or improve visual acuity.
Symptoms
- Objects appear blurry or faded
- Straight lines seem wavy or distorted
- A grey or white spot in the middle of your field of vision
- A dark area obscures the centre of your vision
- Washed-out print when reading

Diagnosis
Optical coherence tomography (OCT) creates detailed images of the different layers of the retina. Safe and non-invasive, it can identify signs of AMD early.
Fluorescein angiography helps your doctor identify wet AMD. The procedure involves injecting a dye into your arm and taking photos of the retina. This should confirm the presence of abnormal blood vessels and identify any leaks or scar tissue.
Dry AMD
Dry AMD is the most common form of macular degeneration. As you age, your macula may become blotchy and pigmented. The process is slow and can have little to no effect on vision. Later, dots called drusen can appear as cells in the macula die off, causing distortion, blurring or missing pieces in images. Most people retain enough vision to function in day-to-day life – although reading and fine detail work may become more difficult.
Treatment
There is no effective treatment for dry AMD at present, but trials are in progress – Auckland Eye is involved with some of these.
Wet AMD
Less common but more serious, wet AMD results from abnormal blood vessel growth on or around the macula. When these blood vessels leak or bleed, the scar tissue left behind can distort and obscure vision. Wet AMD tends to develop more quickly than dry and may lead to severe vision problems and blindness if left untreated. Wet AMD treatment options:
Anti-VEGF injections
The most common treatment for wet AMD is anti-VEGF (vascular endothelial growth factor) injections, which inhibit the growth of new blood vessels in the macula. The treatment effectively prevents or slows vision loss in 90% of patients and improves vision in 60%.
After numbing your eye, your ophthalmologist will inject the drug through the eye’s sclera, or outer layer. This should not be painful but may be uncomfortable. Treatment is ongoing, with injections every month for the first three months, then every three months, depending on how the eye responds.
Laser treatment
Although laser treatment for AMD has been less common since the introduction of anti-VEGF medication, it is still occasionally used. Your ophthalmologist may recommend laser treatment if your AMD doesn’t respond well to the anti-VEGF treatment.
Photodynamic therapy (PDT) involves injecting a special light-sensitive fluid into the arm and using a laser to activate it in the eye and help close off the abnormal blood vessels causing wet AMD.
Laser photocoagulation involves directing a specialised laser at the blood vessels around the macula. As with PDT, the laser blocks the abnormal vessels, which naturally die off.

Preventing macular degeneration
Because most cases of AMD are not treatable, prevention and early detection are the best ways to minimise your risk.
Here’s how:
- Diet and exercise – lowering blood pressure and cholesterol can reduce the risks of AMD.
- Stay smoke-free – smoking is a major risk factor.
- Vitamin supplements – there is some evidence that specific vitamin supplements, including Vitamin A, Vitamin C and lutein can lower your risk of developing late-stage AMD. Ask your ophthalmologist if these are suitable for you.
- Early detection – wet AMD can be treated effectively if caught early. Have regular check-ups with an ophthalmologist and check yourself using the Amsler grid below.
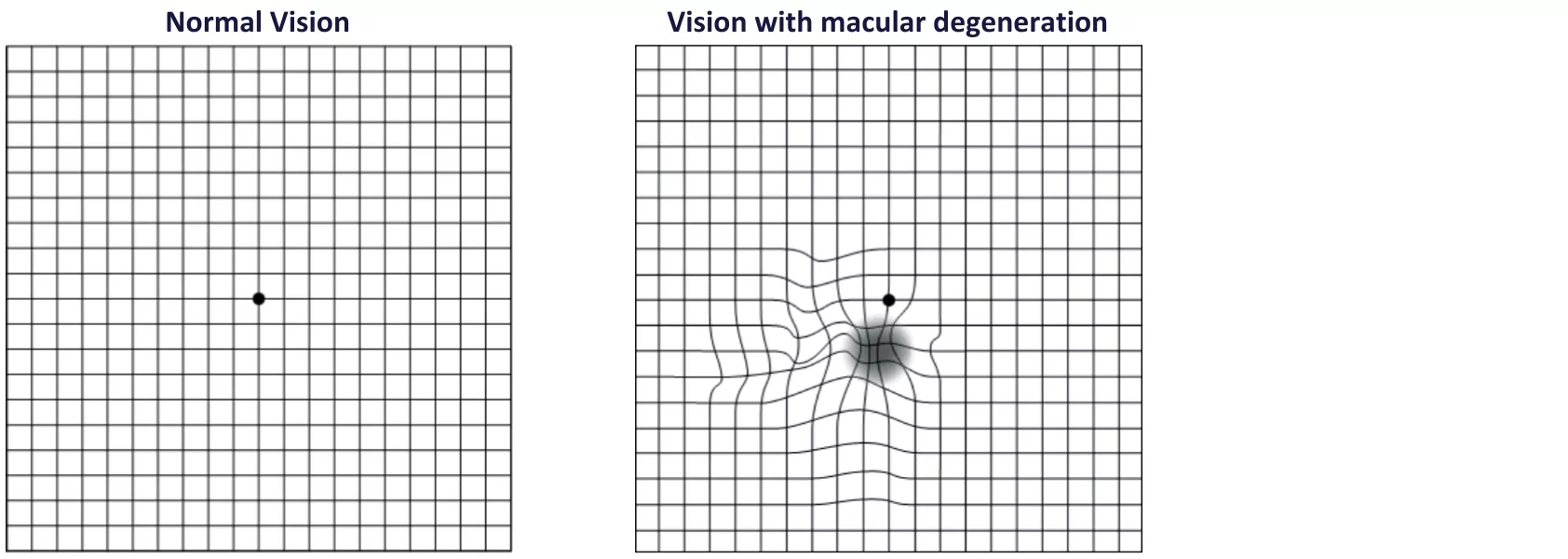
Check for signs with the Amsler grid
The Amsler grid is a simple way to check for early signs of AMD. If you do notice concerning signs, get in touch with your ophthalmologist immediately.
Amsler grid instructions:
- If you wear contact lenses or glasses for reading, put them on for the test.
- In a well-lit space, sit or stand roughly 33cm away from the grid.
- Cover one eye and focus the other eye on the central dot.
- Switch eyes and repeat.
- If lines seem wavy, broken or distorted, or if other parts of the grid seem blurry or missing, seek help from your eye specialist.
Future Development for Treatments
Treatment and techniques to reduce macular degeneration (both the wet and dry form) will be increasingly important as it is a major cause of visual impairment in the developed world, including New Zealand. Auckland Eye actively participates in international clinical trials investigating new drugs for both the treatment and possible prevention of AMD in the future.
Macular Degeneration New Zealand (MDNZ)
MDNZ is a charitable trust with a vision to provide awareness, education and support to those who suffer from the disease. If you would like further information then please contact Macular Degeneration New Zealand:
Web: www.mdnz.org.nz
Tel: 0800 MACULA (0800 622 852).













