Auckland Eye sets new standard in digital accessibility with website toolbar launch
Discover how Auckland Eye is redefining inclusive healthcare by launching New Zealand’s first assistive website toolbar.

Keratoconus (ker-uh-toe-KOH-nus) is a condition estimated to affect as many as 1 in 375 people. It’s an eye disease that alters the quality and shape of your cornea (the clear, usually dome-shaped front surface of your eyeball), causing blurred vision and sensitivity to light and glare. While the exact cause remains unknown, fortunately, treatment options are plentiful and varied depending on the severity of the condition.

With keratoconus, the usually round cornea becomes thin, distorted and cone-shaped. As a result of this irregular shape, it can’t perform its job properly. When this refractive process cannot be carried out correctly, the images passed to the retina and transmitted to the brain become distorted and blurred.

Several factors appear to contribute to keratoconus, but an exact cause is yet to be pinpointed. Genetic and environmental factors are thought to be critical contributors:

Typically developing in the teenage years with progression halting around the age of 30, the symptoms of keratoconus range from mild to severe and can change as the disease progresses. Recent studies have shown that men, African Americans and Latinos are at greater risk, while women, Asian Americans and people with diabetes appear to have a lower risk.
Here are the four most common symptoms:
There are several options available to treat and halt the progress of keratoconus, based on the severity of the condition and the disorder’s progression. The most common forms of treatment are broken into non-surgical and surgical:
Non-surgical
Surgical
Corneal crosslinking
Corneal crosslinking (CXL) is a relatively new treatment option that is quick and less invasive.
Intrastromal corneal ring segments
Clear, arc-shaped implants known as ICRS or Intacs are surgically placed on the outer edge of the cornea to remodel, flatten and create symmetry in the cornea.
This reduces distortion and helps improve vision, but most patients will still require glasses or contact lenses after the treatment.
Corneal transplants
When other treatments are no longer viable options, an eye specialist may recommend a corneal transplant.
Dating back to the early 1900s, a corneal transplant involves replacing a patient’s damaged cornea with healthy donor corneal tissue (the National Eye Bank provides human tissue after careful quality screening).
Different procedures can be used, and the surgery is typically reserved for people with severe keratoconus who can’t tolerate or haven’t responded well to other treatments.
The causes, treatments and diagnostics of keratoconus are continually being researched and developed, and with timely treatment, most people will have good outcomes.
If you’re experiencing any vision issues or suspect you may have keratoconus, booking an appointment is the best thing you can do. Early treatment can help decrease the severity and prevent worsening symptoms.
Auckland Eye is well-equipped with the most advanced technology, knowledge and training to diagnose and treat keratoconus changes to the eye, meaning you’ll benefit from the best possible visual outcomes.
If you have a question or would like to book an appointment, please contact our friendly specialist team on 0800 AKL EYES or email to admin@aucklandeye.co.nz
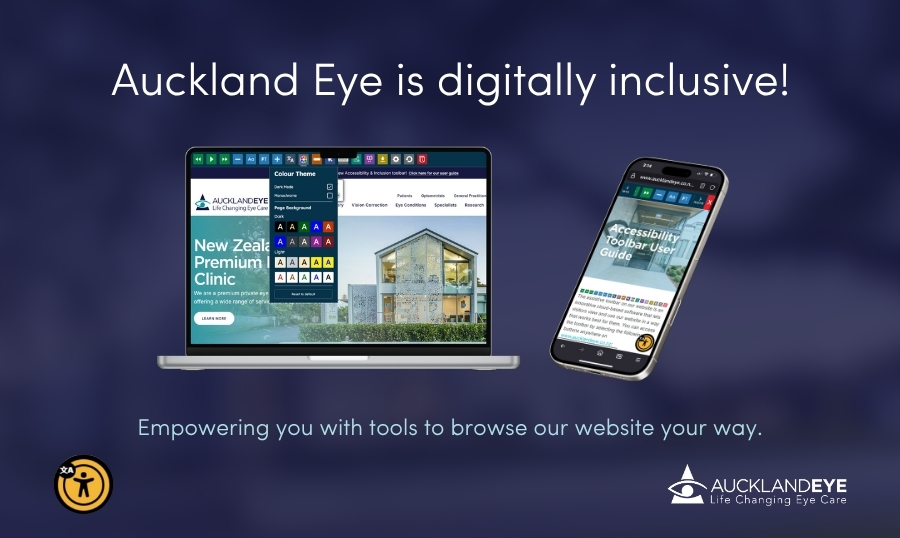
Discover how Auckland Eye is redefining inclusive healthcare by launching New Zealand’s first assistive website toolbar.
Macular degeneration is a leading cause of vision loss in older adults. There’s no cure, but its progression can be slowed. Here’s what to know.

Auckland Eye hosted an extraordinary Continued Medical Education (CME) day titled “Walk in Our Surgeons’ Shoes (Socks)”.