The 5 Most Common Eye Injuries for Athletes
Sports and physical activities play a crucial role in maintaining a healthy lifestyle, but they also come with potential risks, including eye injuries

Today with our exponentially increasing obesity rates, ageing population, urbanisation and emphasis on computer oriented-work and sedentary lifestyles, diabetes and therefore diabetic retinopathy is becoming a major public health problem. It is estimated that currently nearly 10 percent of the world’s adults have diabetes, and the prevalence continues to rise rapidly, so diabetes and diabetic retinopathy are now approaching epidemic proportions everywhere.
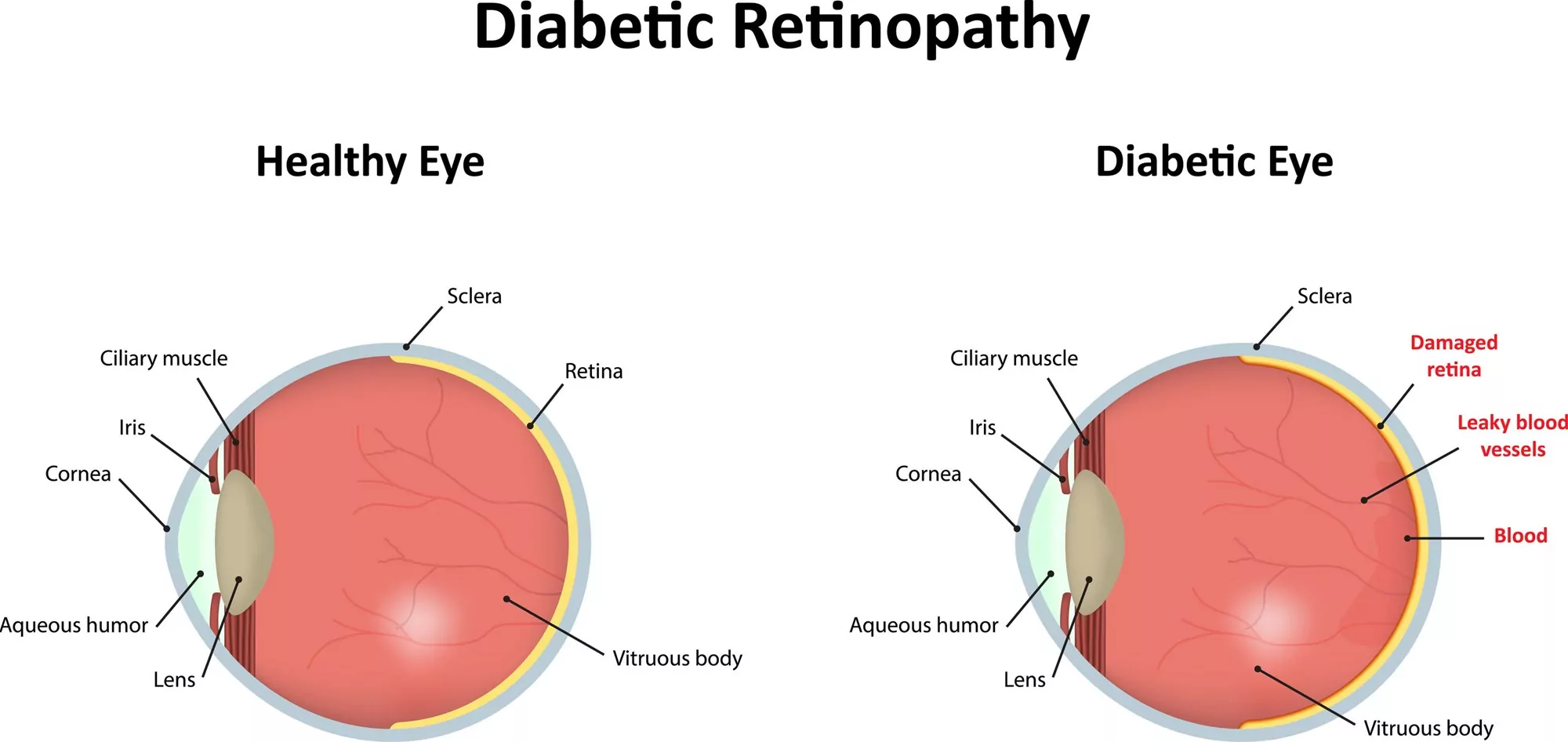
Diabetic retinopathy is the name for damage to the retina (the light-sensitive membrane at the back of the eye that enables vision) caused by diabetes. Diabetes is a chronic disease that occurs when the pancreas is no longer able to make insulin or when the body cannot make good use of the insulin it produces and as a result blood sugar levels rise to dangerous levels. This means that for someone who has diabetes, their body cannot utilise the sugar (glucose), therefore the glucose remains in the blood stream. This sugar reacts with the walls of the blood vessels, and as it does, this causes the cells that line the blood vessels to swell and become damaged.
These blood vessels may leak fluid or bleed into the retina and if the changes are severe they will affect the health of your retina. As the blood vessels become increasingly damaged with poor blood sugar control, they can become completely obstructed, depleting the retina of blood and nutrients. Abnormal new blood vessels may then grow and possibly bleed into the eye cavity, causing severe vision loss.
All people with type 1 or type 2 diabetes are at risk of developing diabetic retinopathy. However, the longer you have been a diabetic the greater the chance of getting this condition. Therefore, people who have had diabetes for over 10 years are more likely to develop diabetic retinopathy. Additionally, pregnant women and those who regularly smoke or have poor control of their blood sugar, cholesterol and blood pressure are at greater risk.
Lifestyle influences including a lack of physical activity, regular smoking and a poor diet comprised of highly processed foods are closely linked with the risks associated with diabetic retinopathy. As a general rule if you have diabetes, we recommend that you adhere to the guidelines indicating when you should pay a visit to visit your eye care specialist:
Type 1 Diabetes: Within 5 years of being diagnosed, then every year thereafter
Type 2 Diabetes: When diagnosed, then annually
During pregnancy: During the first trimester
Based on the severity of your disease or the concern about possible progression of vision loss, your ophthalmologist may need to see you more often.
During an eye exam, the ophthalmologist or optometrist will perform various tests to check the retina to see if there are any haemorrhages or any blood vessels that are leaking fluid into the retinal tissue. Getting treatment for diabetic retinopathy as soon as possible is the best way to prevent future vision loss.
Lifestyle choices play a significant role not only in your general overall health but also your visual health. Maintaining a healthy weight, keeping a healthy balanced diet with limited processed foods and regular exercise can help to manage your blood sugar levels.
Smoking is also a major risk factor for developing diabetic retinopathy and can cause vision loss to progress faster. Even though quitting can be difficult, if you are a smoker we highly recommend that you quit, as the nicotine in tobacco not only contributes to elevated blood pressure and cholesterol, but it also damages insulin activity.

If you have diabetes talk with your GP about keeping your blood sugar levels in-check. Aside from regularly checking your blood sugar levels through the day with a glucometer test, request to have regular HbA1c blood tests when visiting your doctor. HbA1c is a useful monitoring tool which reflects the average blood glucose (sugar in your bloodstream) over the previous 6 weeks. This test gives an indication of your longer-term blood glucose control.
If you have kidney problems or high blood pressure, talk to your doctor about ways to manage and treat these problems. Controlling your high blood pressure and learning how to effectively manage it will help to keep your eyes’ blood vessels healthy.

Taking your medications as prescribed by your doctor is vital to your eye health.
If you notice any changes in your vision in one or both eyes, including flashes of light or many more spots (floaters) than usual, be sure to see an ophthalmologist or optometrist right away.
While diabetic retinopathy can cause significant loss of vision effective management of your blood sugar levels and making a few simple lifestyle changes can help preserve your vision. Most importantly, regular retinal eye examinations can help to detect any abnormalities before any signs or symptoms of retinopathy occur. Early treatment is better for providing a successful outcome and for preserving your sight.
Diabetic patients who have vision problems from retinopathy can usually be successfully managed with laser and/or other treatment options.
To find out more about diabetic retinopathy and the treatments we offer here at Auckland Eye, visit: https://www.aucklandeye.co.nz/eye-conditions/diabetic-retinopathy/

Sports and physical activities play a crucial role in maintaining a healthy lifestyle, but they also come with potential risks, including eye injuries

For those leading an active lifestyle or engaged in sports, the significance of clear vision cannot be overstated.

Uncover the revolutionary technology behind LASIK that has empowered millions to enjoy clear vision without glasses.